Singapore has one of the world’s highest diabetes rates. With diabetes often comes other issues that may affect their overall health. For instance, obesity and hypertension are closely associated with diabetes. Likewise, a person with diabetes may also have gum disease.
The relationship between gum disease and diabetes is bi-directional. This means that not only are patients with diabetes more prone to periodontitis, but periodontitis can also make it harder for them to control their blood sugar levels. In the United States, diabetics have been shown to be 4.2 times more likely to develop bone loss due to periodontitis than those without diabetes.

Gum Disease: Gingivitis vs Periodontitis
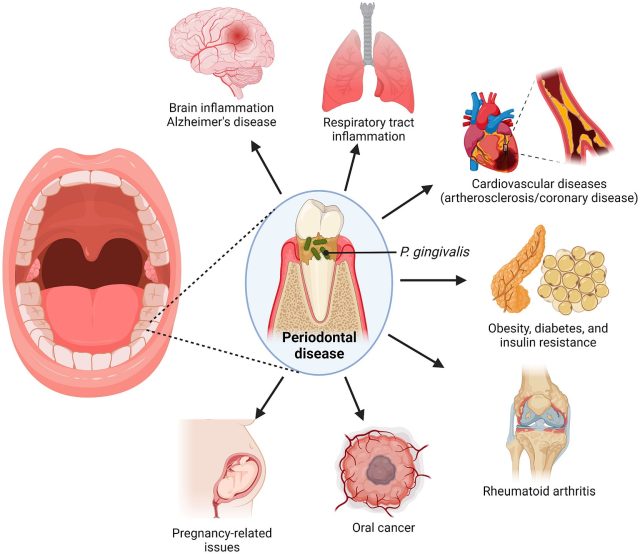
Periodontal disease, commonly called gum disease, is a chronic bacterial infection affecting the gums. It begins with the buildup of plaque, a sticky film of bacteria that constantly forms on the teeth.
In the early stage of gum disease, called gingivitis, the bacteria in plaque release toxins that irritate and inflame the gums, causing redness and swelling. However, sometimes the gums may appear normal despite the presence of gingivitis.
If left untreated, the disease progresses to periodontitis, where the toxins produced by the bacteria start to destroy the bone that supports the teeth. Although periodontitis is often painless in its early stages, symptoms such as gum swelling, pain, and tooth loosening may develop as the disease worsens.
Gum Disease and Diabetes
Diabetes can impair white blood cells, crucial for fighting infection, and reduce collagen levels necessary for gum health and healing. This impairment is more pronounced in individuals with poorly controlled diabetes, making them more susceptible to gum disease and hindering their ability to recover.
Moreover, the severity of periodontitis tends to increase in patients with diabetes with advanced complications or a longer duration of the disease. Conversely, well-controlled diabetics face a lower risk of gum disease compared to those with poorly managed diabetes.
Note that individuals with uncontrolled or poorly controlled diabetes may experience other oral discomfort, such as a burning sensation in the mouth or tongue, often attributed to reduced saliva flow. They may also be more susceptible to tooth decay and fungal infections.
Gum Disease and Diabetes: Things to Know About Treatment and Dental Care
Successful treatment of gum disease in individuals with diabetes involves a collaborative approach between the periodontist and the patient’s physician or endocrinologist, especially if the diabetes is poorly controlled.
The periodontist requires essential medical information, including the patient’s blood sugar levels and current medications. This information helps tailor the treatment plan to the individual’s needs.
The periodontal treatment strategy may need adjustments based on the patient’s medications and the level of diabetes control. This ensures that treatment is safe and effective.
For Well-Controlled Diabetes:
In cases of well-controlled diabetes, the gum disease treatment generally follows a similar approach to that for non-diabetic patients, unless other medical conditions are present.
Patients should continue taking their prescribed medications and maintain a normal diet, including a healthy breakfast before appointments. Early morning appointments are often preferred due to higher levels of a stress-reducing hormone at that time.
For Poorly Controlled Diabetes:
For individuals with poorly controlled diabetes, collaboration with their physician or endocrinologist is crucial. While gum treatment is still recommended, these patients might not respond as favourably as those with well-controlled diabetes. However, research suggests that effectively managing periodontitis in poorly controlled diabetics may contribute to improved blood sugar control.
In general, the standard treatment for gum disease typically involves multiple sessions of deep scaling beneath the gums, usually performed under local anaesthesia. In certain cases, surgical intervention might be necessary. Additionally, periodontal treatment can be combined with treatments from other dental specialties if tooth replacement is required.
Periodontal Disease Link with Osteoporosis
Currently, there is a weak association between osteoporosis and gum disease. This means that we are still uncertain about how osteoporosis influences bone loss in periodontitis (gum disease), although a link seems to exist. Importantly, gum disease does not cause osteoporosis.
Past studies suggest osteoporosis might contribute to tooth loss due to decreased bone density supporting the teeth, and hormone replacement therapy may offer some protection. Further research is ongoing to clarify and substantiate this connection.
Osteoporosis Oral Health
Medications used to treat osteoporosis, such as Fosamax (a bisphosphonate) Aclasta, and the like, can have dental implications. Patients taking Fosamax or similar drugs have a slightly increased risk of osteonecrosis (jawbone destruction) if they undergo extraction or oral surgery.
Therefore, individuals on Fosamax should prioritise regular dental checkups and maintenance to prevent the need for extractions or surgery. Doctors often refer patients for dental clearance before starting this medication.
Maintaining healthy gums and teeth is crucial, as the onset of osteoporosis, especially in women, is unpredictable. If periodontal disease cannot be controlled before starting the medication, extractions might be necessary. Regular gum checks can help avoid tooth loss in such situations. Remember, losing teeth as we age is a misconception.
Dental Care and Healthy Gums: What Can You Do?
Prevention is always the best approach, especially when managing interconnected conditions like gum disease and diabetes. Optimal oral health, which can significantly impact both conditions, can be achieved through:
- Good control of diabetes: Effective management of diabetes through medication, diet, and exercise as advised by your doctor is crucial. This not only helps in controlling blood sugar levels but also reduces the risk of gum disease and its potential impact on bone health.
- Regular dental check-ups: Routine dental examinations, including gum checks and X-rays, are essential for early detection and treatment of gum disease.
- Regular scaling or periodontal maintenance: Professional cleaning by a dentist or periodontist helps remove plaque and tartar buildup, reducing the risk of gum disease progression and its potential complications for bone health.
Conclusion
Periodontal disease link with diabetes and osteoporosis necessitates a comprehensive approach to healthcare. Effective diabetes management, coupled with regular dental check-ups and meticulous oral hygiene, plays a pivotal role in mitigating the risks and complications associated with these interconnected conditions.
References:
Diabetes and periodontitis: How well are the patients aware about an established relation? – PMC, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5341327/ Accessed October 12, 2024
View of Managing Periodontitis in Type 1 Diabetic Patients Improves Glycemic Control: A Case Report. , https://www.asean-endocrinejournal.org/index.php/JAFES/article/view/321/763#:~:text=Treatment%20of%20periodontal%20disease%20has,in%20HbA1c%20in%20diabetic%20patients Accessed October 12, 2024
Diabetes, Gum Disease, & Other Dental Problems – NIDDK , https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/gum-disease-dental-problems Accessed October 12, 2024

